*/
Richard Jones QC meets the President of the Royal College of Paediatrics and Child Health, Professor Terence Stephenson
Unsurprisingly, child protection is a hot topic for paediatricians. Suspect child abuse when it didn’t happen or miss child abuse when it did happen – both invite public criticism. Professor Terence Stephenson is the President of the Royal College of Paediatrics and Child Health and he talked to Counsel about his profession’s role in such cases. He also discussed some of his perceptions about our own profession operating in cases involving children, whether in the Crown Court or a family court. He brings his own experience of appearing in over 50 cases during the past 25 years.
Consider two case scenarios. A clinician may be concerned that a child is suffering from meningitis. He prescribes antibiotics and decides the child should have a lumbar puncture. A couple of days later it turns out to be a false alarm and the child is discharged. It is highly likely that there will not be any parental reaction except gratitude for the taking of appropriate precautions.
Next take the case where a child has an unusual pattern of bruising. The clinician then acts upon what is only a suspicion (and that is what they properly do act upon) that there has been non-accidental injury. The parent is not accused of carrying out any acts of violence, but they are told that the local authority children’s services have been alerted and that the police may have to be informed. A few days later, after appropriate investigation, the conclusion is reached that there is no cause for concern and the child is discharged. It is likely that the parent will be aghast that such implicit criticism is being made and may well take matters further by way of some form of complaint. Such strong reactions can of course create a defensive mindset. Professor Stephenson states that there was a recent survey in a UK Accident & Emergency department. It emerged that only 50 per cent of cases were being reported where concern had been raised by clinicians about possible non-accidental injury.
The role of the paediatrician as expert witness has come under the microscope on a number of occasions in recent years, and paediatricians have not always emerged in a positive light. Professor Sir Roy Meadow and Professor David Southall became household names as a result of the evidence they gave or views they formed, and both were the subject of disciplinary proceedings and – at least – initially were struck off the medical register (both are now reinstated).
One major difficulty encountered by his profession, Professor Stephenson observes, is that the majority of paediatricians are increasingly unwilling to act as an expert witness. When travelling round the country, visiting paediatricians as part of his role as President of the Royal College of Paediatrics and Child Health, this has been a recurrent theme. Why? The reasons, he says, are obvious.
Over the past ten years or so, the perception is that a paediatrician who gives unfavourable evidence as an expert is at risk of being the subject of a complaint to the General Medical Council. Even if that complaint is unjustified, it is not a pleasant prospect for anyone. Additionally, it is far from unknown for there to be a degree of vilification of such experts, harassment and adverse comments in the press. Put these together, and the reluctance of paediatricians to give expert evidence is unsurprising. Of the 3,000 or so paediatric consultants in the country, Professor Stephenson estimates that there are less than 100 who are prepared to give expert evidence in child protection cases. Even that pool continues to reduce in size. Solicitors operating in this field complain bitterly about the paucity of available persons to instruct.
A clear distinction can be drawn with treating clinicians and experts. The expert is obviously in a very different position. He is unlikely to have seen the child in question, and will be basing his opinion upon X-rays, reports and documentation completed by others.
Part of the problem, says Professor Stephenson, is that he believes insufficient support has been offered by the authorities to those who give expert evidence, especially since the vast majority of such persons deliver a first class service. The judiciary too, he believes, could play its part in ensuring that the expert is not personally undermined.
Recognising these difficulties, the Chief Medical Officer proposed, in his discussion document “Bearing Good Witness”, a network of clinicians providing mentoring, supervision and peer review of experts within a local group. This can give rise to a collective view formed by the group after scrutiny of the relevant materials, giving comfort and support to the individual who gives evidence. The risk of course is that the expert may be accused of not forming an independent view, but has been influenced by others. Another perception on the part of parents may be that since the experts all tend to be employed by the NHS, there is a risk of lack of independence. “Bearing Good Witness” was published in 2006. The consultation ended in February 2007 and little has happened since then to take it forward.
Another issue raised by Professor Stephenson is that of the style of some advocates. He well recognises the need for fair challenges to disputed evidence, and acknowledges that the industry and application of opposing teams in cases in which he has himself been involved have caused him to reconsider his own views. But, and it is a big but, some styles of cross-examination can stray from the merely confrontational into an attack (or perceived attack) on the witness’s personal integrity.
Why does this occur? It may be due to a number of factors. Who has not felt pressure from the lay or professional client? Added to that is the nature of the evidence, the risks of adverse findings and the dire consequences which may flow from such findings. But it has made a number of paediatric experts feel less than comfortable and indeed metaphorically they consider giving evidence to have been a bruising experience. And that in turn makes them less likely to want to repeat the experience and makes the pool of available experts that much smaller.
Professor Stephenson seeks no favours from the Bar, and indeed it is fair to say that experts in other fields are frequently the subject of forceful challenge. However, there are, he believes, ways for advocates to make it plain that while attacking the conclusions of a particular expert, such an attack does not extend to a challenge to their personal integrity. From the point of view of the Royal College, which has training responsibilities, it provides (and they are over-subscribed) training programmes in child protection for those who may be called upon to give child protection evidence in court, helped by members of the Bar acting pro bono. Such courses can also prepare potential experts for giving evidence in hostile circumstances.
On a positive note, Professor Stephenson praises the case management processes which are now in place which lead to significant reductions in witnesses waiting to be called. He notes the new processes for consideration of expert evidence (and in particular the narrowing of issues) in criminal proceedings following the Court of Appeal’s ruling in R v Henderson [2010] EWCA Crim 1269 which many consider to be most helpful in focussing attention on the real issues in any particular case.
In conclusion, Professor Stephenson stresses that he is in no way trying to stop paediatricians being given a hard time in court, or suggesting that their critical evidence should not be tested. But it is a fair point to make that a consequence of inappropriate cross-examination could be that paediatricians will stop acting as expert witnesses.
Richard Jones, No5 Chambers, is the Chairman of Counsel’s Policy and Editorial Board
The College is a charity established by Royal Charter. Founded in 1996, it is one of the Medical Royal Colleges. Like the other Colleges, it plays a major role in postgraduate medical education and professional standards: setting syllabuses for postgraduate training in paediatrics, overseeing the training, running examinations, organising courses and conferences, issuing guidance and conducting research. It currently has over 11,000 members both in the UK and overseas. For further information visit www.rcpch.ac.uk
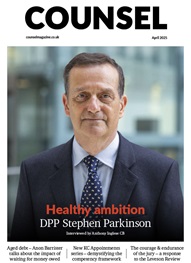
Professor Terence Stephenson DM, FRCP, FRCPCH
Professor Stephenson became President of the Royal College of Paediatrics and Child Health in April 2009. He is also Nuffield Professor of Child Health at the Institute of Child Health, University College London.
Professor Stephenson is a consultant in general paediatrics and his research reflects his clinical interests in paediatric medicine and paediatric emergencies. He has co-authored textbooks, written numerous invited chapters and editorials, and published over 120 peer reviewed papers.
Unsurprisingly, child protection is a hot topic for paediatricians. Suspect child abuse when it didn’t happen or miss child abuse when it did happen – both invite public criticism. Professor Terence Stephenson is the President of the Royal College of Paediatrics and Child Health and he talked to Counsel about his profession’s role in such cases. He also discussed some of his perceptions about our own profession operating in cases involving children, whether in the Crown Court or a family court. He brings his own experience of appearing in over 50 cases during the past 25 years.
Consider two case scenarios. A clinician may be concerned that a child is suffering from meningitis. He prescribes antibiotics and decides the child should have a lumbar puncture. A couple of days later it turns out to be a false alarm and the child is discharged. It is highly likely that there will not be any parental reaction except gratitude for the taking of appropriate precautions.
Next take the case where a child has an unusual pattern of bruising. The clinician then acts upon what is only a suspicion (and that is what they properly do act upon) that there has been non-accidental injury. The parent is not accused of carrying out any acts of violence, but they are told that the local authority children’s services have been alerted and that the police may have to be informed. A few days later, after appropriate investigation, the conclusion is reached that there is no cause for concern and the child is discharged. It is likely that the parent will be aghast that such implicit criticism is being made and may well take matters further by way of some form of complaint. Such strong reactions can of course create a defensive mindset. Professor Stephenson states that there was a recent survey in a UK Accident & Emergency department. It emerged that only 50 per cent of cases were being reported where concern had been raised by clinicians about possible non-accidental injury.
The role of the paediatrician as expert witness has come under the microscope on a number of occasions in recent years, and paediatricians have not always emerged in a positive light. Professor Sir Roy Meadow and Professor David Southall became household names as a result of the evidence they gave or views they formed, and both were the subject of disciplinary proceedings and – at least – initially were struck off the medical register (both are now reinstated).
One major difficulty encountered by his profession, Professor Stephenson observes, is that the majority of paediatricians are increasingly unwilling to act as an expert witness. When travelling round the country, visiting paediatricians as part of his role as President of the Royal College of Paediatrics and Child Health, this has been a recurrent theme. Why? The reasons, he says, are obvious.
Over the past ten years or so, the perception is that a paediatrician who gives unfavourable evidence as an expert is at risk of being the subject of a complaint to the General Medical Council. Even if that complaint is unjustified, it is not a pleasant prospect for anyone. Additionally, it is far from unknown for there to be a degree of vilification of such experts, harassment and adverse comments in the press. Put these together, and the reluctance of paediatricians to give expert evidence is unsurprising. Of the 3,000 or so paediatric consultants in the country, Professor Stephenson estimates that there are less than 100 who are prepared to give expert evidence in child protection cases. Even that pool continues to reduce in size. Solicitors operating in this field complain bitterly about the paucity of available persons to instruct.
A clear distinction can be drawn with treating clinicians and experts. The expert is obviously in a very different position. He is unlikely to have seen the child in question, and will be basing his opinion upon X-rays, reports and documentation completed by others.
Part of the problem, says Professor Stephenson, is that he believes insufficient support has been offered by the authorities to those who give expert evidence, especially since the vast majority of such persons deliver a first class service. The judiciary too, he believes, could play its part in ensuring that the expert is not personally undermined.
Recognising these difficulties, the Chief Medical Officer proposed, in his discussion document “Bearing Good Witness”, a network of clinicians providing mentoring, supervision and peer review of experts within a local group. This can give rise to a collective view formed by the group after scrutiny of the relevant materials, giving comfort and support to the individual who gives evidence. The risk of course is that the expert may be accused of not forming an independent view, but has been influenced by others. Another perception on the part of parents may be that since the experts all tend to be employed by the NHS, there is a risk of lack of independence. “Bearing Good Witness” was published in 2006. The consultation ended in February 2007 and little has happened since then to take it forward.
Another issue raised by Professor Stephenson is that of the style of some advocates. He well recognises the need for fair challenges to disputed evidence, and acknowledges that the industry and application of opposing teams in cases in which he has himself been involved have caused him to reconsider his own views. But, and it is a big but, some styles of cross-examination can stray from the merely confrontational into an attack (or perceived attack) on the witness’s personal integrity.
Why does this occur? It may be due to a number of factors. Who has not felt pressure from the lay or professional client? Added to that is the nature of the evidence, the risks of adverse findings and the dire consequences which may flow from such findings. But it has made a number of paediatric experts feel less than comfortable and indeed metaphorically they consider giving evidence to have been a bruising experience. And that in turn makes them less likely to want to repeat the experience and makes the pool of available experts that much smaller.
Professor Stephenson seeks no favours from the Bar, and indeed it is fair to say that experts in other fields are frequently the subject of forceful challenge. However, there are, he believes, ways for advocates to make it plain that while attacking the conclusions of a particular expert, such an attack does not extend to a challenge to their personal integrity. From the point of view of the Royal College, which has training responsibilities, it provides (and they are over-subscribed) training programmes in child protection for those who may be called upon to give child protection evidence in court, helped by members of the Bar acting pro bono. Such courses can also prepare potential experts for giving evidence in hostile circumstances.
On a positive note, Professor Stephenson praises the case management processes which are now in place which lead to significant reductions in witnesses waiting to be called. He notes the new processes for consideration of expert evidence (and in particular the narrowing of issues) in criminal proceedings following the Court of Appeal’s ruling in R v Henderson [2010] EWCA Crim 1269 which many consider to be most helpful in focussing attention on the real issues in any particular case.
In conclusion, Professor Stephenson stresses that he is in no way trying to stop paediatricians being given a hard time in court, or suggesting that their critical evidence should not be tested. But it is a fair point to make that a consequence of inappropriate cross-examination could be that paediatricians will stop acting as expert witnesses.
Richard Jones, No5 Chambers, is the Chairman of Counsel’s Policy and Editorial Board
The College is a charity established by Royal Charter. Founded in 1996, it is one of the Medical Royal Colleges. Like the other Colleges, it plays a major role in postgraduate medical education and professional standards: setting syllabuses for postgraduate training in paediatrics, overseeing the training, running examinations, organising courses and conferences, issuing guidance and conducting research. It currently has over 11,000 members both in the UK and overseas. For further information visit www.rcpch.ac.uk
Professor Terence Stephenson DM, FRCP, FRCPCH
Professor Stephenson became President of the Royal College of Paediatrics and Child Health in April 2009. He is also Nuffield Professor of Child Health at the Institute of Child Health, University College London.
Professor Stephenson is a consultant in general paediatrics and his research reflects his clinical interests in paediatric medicine and paediatric emergencies. He has co-authored textbooks, written numerous invited chapters and editorials, and published over 120 peer reviewed papers.
Richard Jones QC meets the President of the Royal College of Paediatrics and Child Health, Professor Terence Stephenson

Now is the time to tackle inappropriate behaviour at the Bar as well as extend our reach and collaboration with organisations and individuals at home and abroad
A comparison – Dan Monaghan, Head of DWF Chambers, invites two viewpoints
And if not, why not? asks Louise Crush of Westgate Wealth Management
Marie Law, Head of Toxicology at AlphaBiolabs, discusses the many benefits of oral fluid drug testing for child welfare and protection matters
To mark International Women’s Day, Louise Crush of Westgate Wealth Management looks at how financial planning can help bridge the gap
Casey Randall of AlphaBiolabs answers some of the most common questions regarding relationship DNA testing for court